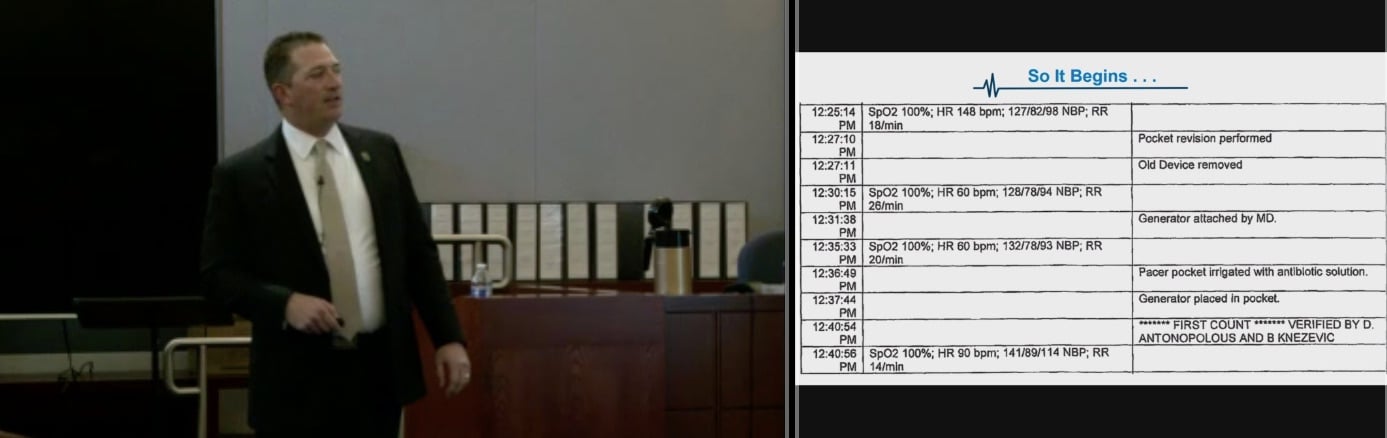
CVN screenshot of plaintiff attorney Sean Claggett walking jurors through a chart of plaintiff Elisa Sales' deteriorating vital signs during his opening statement
Las Vegas, NV - A supposed failure to begin timely resuscitation efforts during an outpatient procedure deprived a woman’s brain of oxygen for nine minutes, leaving her with the mental capacity of a five-year-old, her attorney told a Nevada state court jury on Wednesday.
Attorney Sean Claggett of the Claggett & Sykes Law Firm told jurors that negligence by doctors and staff at Summerlin Hospital during what should have been a routine replacement of plaintiff Elisa Sales’ internal pacemaker and defibrillator in 2016 resulted in injuries warranting damages in the “10’s of millions” plus nearly $8 million just for future medical care.
Sales suffered a severe drop in blood pressure followed by cardiac arrest during a pacemaker replacement. Claggett told jurors her blood pressure dropped because of being given too much of the sedative Propofol, and that doctors failed to begin CPR soon enough due to the audible alarms on nearby vital sign monitors being turned off.
Summerlin Hospital maintains their resuscitation efforts began as soon as Sales began to deteriorate, and they argue her brain injuries are the result of medical conditions predating her pacemaker replacement.
The full trial is being webcast and recorded gavel-to-gavel by Courtroom View Network.
Claggett described to jurors how an anesthesiologist administered a dose of the drug propofol to Sales after the new pacemaker was implanted in order to carry out a test of the device that is extremely painful if the patient is awake.
Claggett claimed the dose was excessive, causing Sales’ vital signs to immediately drop and the anesthesiologist to remark, “I guess she didn’t like the propofol.”
Walking jurors through a minute-by-minute timeline of Sales’ vital signs, Claggett noted her pulse and blood pressure dropping to levels that he said should have begun immediate emergency resuscitation, but allegedly all the audible alarms in the cardiac catheterization lab where the procedure was taking place had been turned off.
“There was no safety net there if the people in that room didn’t do their job,” he said.
One of the physicians present eventually noticed Sales’ crashing vital signs and supposedly asked, “Has anybody checked for a pulse?” CPR began and while Sales’ heart was restarted, Claggett told jurors that nine minutes without oxygen left her with a permanent, disabling hypoxic brain injury requiring a lifetime of constant care.
He argued Summerlin Hospital is responsible both for the failure to adequately train its staff in emergency resuscitation, and for failing to ensure the audible alarms on the vital sign monitors were turned on.
Claggett told jurors that in a deposition the head of Summerlin’s cardiology department said he was unaware of a policy requiring the audible alarms on monitors to be turned on.
“If he doesn’t know, how is anybody below him going to know,” Clagget asked.
He said Summerlin’s stated policies on emergency resuscitation clearly showed CPR should have started sooner for Sales, noting that the guidelines require emergency resuscitation to begin once a patient’s vitals drop below a certain threshold.
“It’s black and white,” he said. “It’s dirt simple. And the evidence will prove in this case they did not follow that policy.”
Representing Summerlin Hospital, Michael Prangle of Hall Prangle and Schoonveld told the jury the resuscitation carried out during Sales’ procedure fell squarely within the standard of care.
“The idea that six medically-trained people literally just sat there for nine minutes simply is not true,” he said.
Prangle argued that for a period of the nine minutes in question Sales did have dangerously low blood pressure (which he said is an expected side effect of Propofol) but still had a pulse.
He described to jurors how the medical team immediately began treatments like administering stimulants and additional fluids after Sales’ blood pressure dropped, but he said starting CPR at that point would not have been consistent with the standard of care.
“You don’t do chest compressions for a low blood pressure,” Prangle said. “You do chest compressions for no pulse.”
Prangle characterized Sales as a “medically fragile person” and suggested that if her brain actually had been deprived of oxygen for nine minutes she would have died.
Prangle rejected the claim Sales suffered a hypoxic brain injury due to lack of oxygen during the procedure, arguing that years of poor blood flow to the brain due to heart disease and diabetes caused her current impairment, which Prangle suggested isn’t as severe as Claggett described.
The trial is taking place before Judge David Jones and is expected to take up to a month to complete, with the full proceedings webcast and recorded gavel-to-gavel by CVN.
The case is captioned Elisa Sales v. Summerlin Hospital and Medical Center, case number A-17-758060-C in the 8th District Court of Nevada, Clark County.
E-mail David Siegel at dsiegel@cvn.com